Are you looking for...
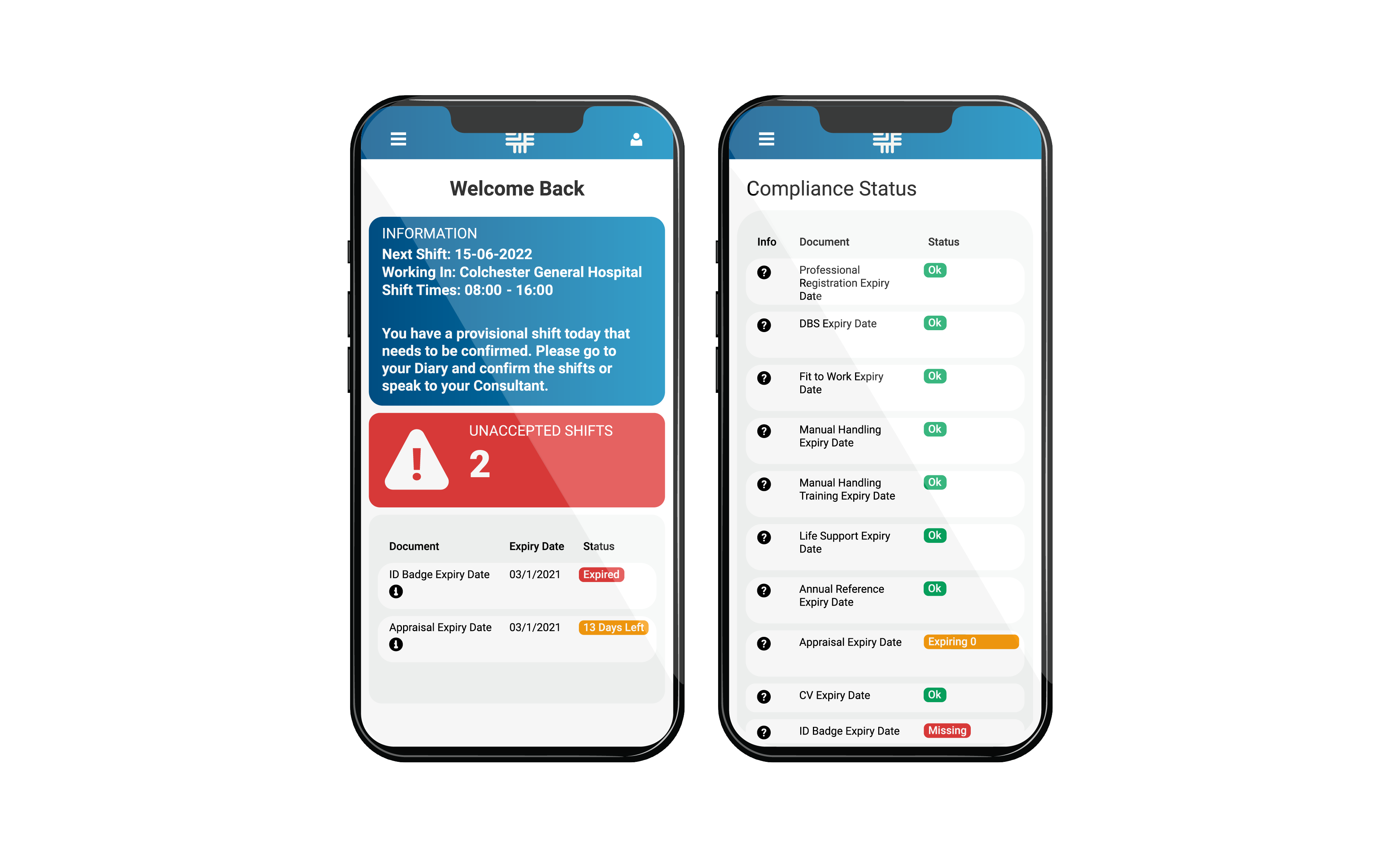
Registerfor our App
Get the work life balance you want. Use the diary, submit your timesheets, & manage your compliance
Here at MedicsPro, we put you first.
As a top-tier agency, we have access to NHS and Private hospitals all over the UK.
This means access to high rates and excellent chances for you to progress your career.